A former St. Albertan is behind a new low-cost diagnostic tool that can quickly indentify those infected by the Zika virus.
Keith Pardee, who grew up in St. Albert and attended Paul Kane High School, is one of the lead authors of a new method, published in the scientific journal Cell Friday, that would allow health professionals to test for the mosquito-borne virus in just a few hours and without the use of electricity or expensive lab equipment.
“What we’re hoping, when this is a product and available, is that it could help identify (infected) people sooner,” said Pardee, “so that they can seek help and the care they need, and to help slow the spread, because as soon as you’re infected, you’re now the source for the next (round of infection).”
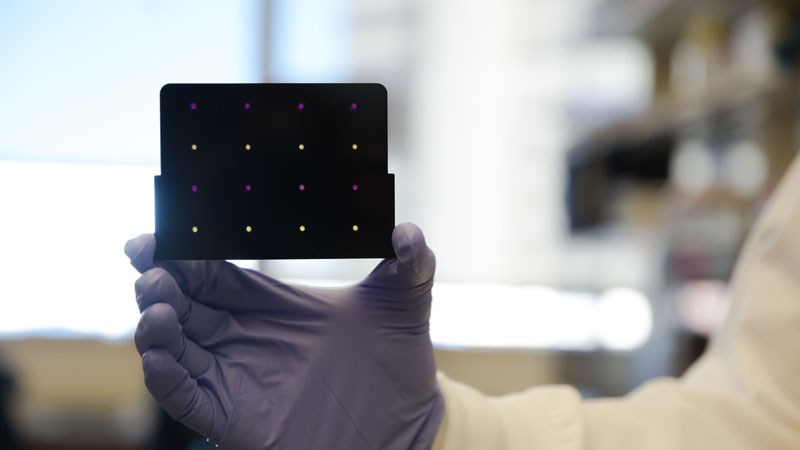
The paper-based test works similarly to a pH paper, but rather than a chemical reaction, Pardee found a way to embed a biological reaction into the paper strips. Using molecular diagnostics, the test looks for specific genetic material – changing colour when present in a person’s blood, urine or saliva.
The RNA sensors are freeze-dried on to the paper strips, allowing for easy and low cost distribution and storage – the tests can be stored at room temperature for up to a year. They are also inexpensive to manufacture, costing between 60 cents and $1.
The speed, ease, portability and low cost of the test makes it the perfect tool for rural, remote or lower income areas, as well as when dealing with outbreaks and pandemics.
In the case of Zika, the test is more accurate than a traditional serology test, which detects antibodies in a patient’s blood serum, given related viruses often cause the body to produce similar antibodies.
“For people who have been exposed to dengue before there is a high likelihood that they will test positive for Zika,” said Pardee.
While a polymerase chain reaction, or PCR, would be more effective in detecting Zika, the method requires expensive equipment, trained lab technicians and the use of electricity.
“We see our test filling that role in a portable way,” said Pardee. “It’s not PCR, but it’s equivalent information in a portable way.”
Pardee has been perfecting the technology for the past two years. Developed in 2014, during his time a post doctorate fellow at the Harvard’s Wyss Institute, the test needed some refining to make it more practical and more sensitive.
But when the Zika outbreak was reported, a team of seven Canadian and American institutions was assembled to get the diagnostic tool market ready as quickly as possible.
“It was the catalyst that probably compressed a year’s worth of work into six weeks,” said Pardee.
The programmability of the sensors was also improved during this time to allow for the detection of the virus strain – Asian, African or American.
“That’s important because of the nature of the American strain. This is something that people are still working out, but it seems to have rare, but more severe, symptoms,” said Pardee.
The U.S. Center for Disease Control confirmed last month that the Zika virus is a cause of microcephaly – a birth defect where babies are born with abnormally small heads. The virus has also been linked to Guillain-BarrĂ© syndrome, a rare disorder that causes the body’s immune system to attack the nervous system.
The diagnostic method is not yet available as a testing kit, but the academic team is hopeful a partner will sign on soon so that their technology can be manufactured and delivered to affected communities.
“We’re hopeful it could be (available for distribution) in a matter of months,” said Pardee.